Phenotyping Core
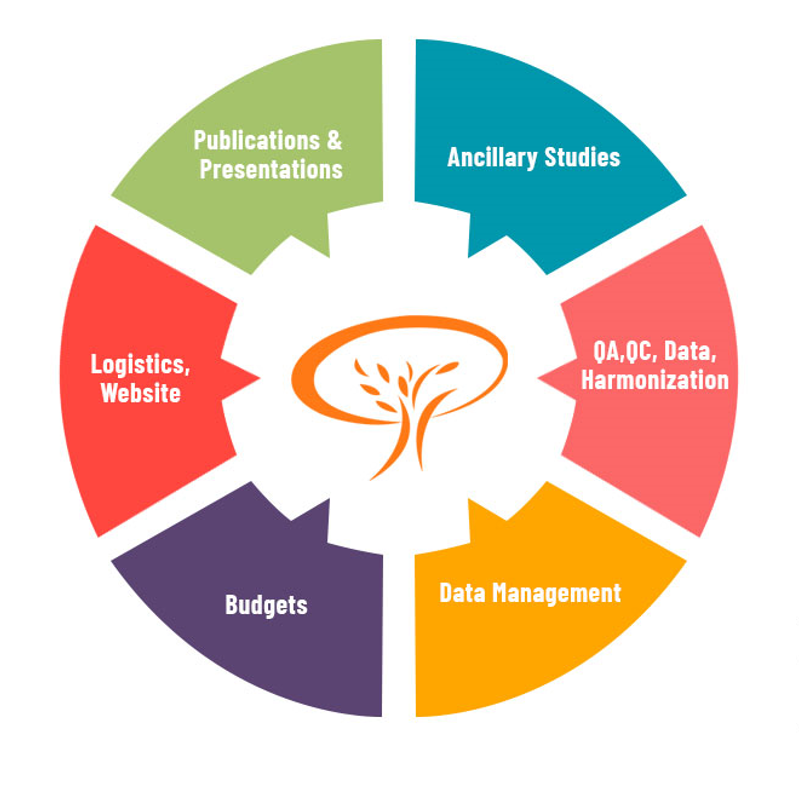
Overview
Co-PIs: Drs. Anne B Newman and Thomas Perls
The LLFS Phenotyping Core efforts are integral to discovering genetic and other factors that predispose to Exceptional Longevity (EL) and health span. The Phenotyping Core is responsible for the development, implementation of and adherence to protocols related to interaction with study participants. Activities include coordination of in-person collection of phenotypic data and biospecimens during the third in-person visit (Visit 1 occurred 2006-2009, Visit 2 during 2014-2017), insuring consistent and reproducible data collection via research assistant standardized training and testing, annual collection of follow-up data, processing data post-collection and determination and collection of missing data, collection of medical records and death certificates, physician follow-up with participants for medical and laboratory alerts, Alzheimer’s disease (AD) and dementia review panel, cause-of-death consensus committee meetings and data harmonization between the LLFS and other studies including Framingham Heart Study (FHS), and new to the LLFS, Baltimore Longitudinal Study of Aging (BLSA) and New England Centenarian Study (NECS).
The previous in-person exams, performed ~8 years apart, identified families demonstrating clustering of individuals with exceptional memory, grip strength, pulmonary function, blood pressure, and/or metabolism. These “healthy aging phenotypes” (HAPs) likely signify different underlying mechanisms for achieving exceptional longevity. Continued prospective study of LLFS participants will determine which individuals are truly exceptional in terms of these HAPs, their rates of change & their relationships to EL.
Longitudinal study has been critical for characterizing rates-of-change in aging-related phenotypes, and this will be even more the case during Visit 3 as the offspring generation enters into ages where we expect to capture aging-related changes. Furthermore, the last of our older generation participants will likely pass away in the next five years and it’s important that we identify terminal decline and other evidence (or lack thereof) of compression of morbidity that has been noted to be prevalent in the extremely old. The addition of omics will allow us to discover preclinical phenotypic changes as well as tremendously expand the measures that may lead to the discovery of pathways and potential therapeutic/prevention targets affecting HAPs and EL.
Aim 1
In service to Project 1 Aim P1, we will conduct a third in-person examination (Visit 3) on all surviving LLFS participants to collect physical and cognitive function measures and biomaterial as well as to continue to collect annual follow-up data via mailed questionnaires and telephone interviews. In addition, for the first time, we will enroll and study 826 participants from the grandchild generation (G3) from 41 families that show the strongest support for linkage for various HAPs.
Aim 2
A new Dementia Review Panel will be added to enable the research diagnoses of probable Alzheimer’s disease (AD) and other dementias in order to aid with Project 1 Aim P1a. LLFS offspring less frequently demonstrate the cognitive profile of AD than spouse controls and some LLFS families exhibit a cognitive HAP. In part from this evidence, we suspect that some LLFS families demonstrate resistance to AD. Assessing for AD will allow LLFS and other investigators to search for omics-derived factors and signatures associated with reduced risk of AD and dementia, resistance to such conditions in the presence of risk factors (e.g., APOE), and with new clinical-neuropathological correlation findings.
Aim 3
To ensure replication and validation opportunities, the Phenotyping Core will conduct data harmonization efforts with the Baltimore Longitudinal Study on Aging (BLSA) and the New England Centenarian Study (NECS) while also adding to such efforts already performed with Medicare and the Framingham Heart Study (FHS) (e.g. digital data measures) in collaboration with the Administrative Core.
Field Operations Committee
The Field Operations committee deals with the logistical issues of the in-person exams and the annual telephone and mail follow-up. Responsible for creating the protocol for the third in-person exam, recruitment of grandchildren, and continuing annual follow-up with LLFS participants. All the phenotypic reading centers are organized under the direction of the Field Operations Committee. The committee is also responsible for putting together the Manual of Procedures (MOP) for all in-person data being collected. Oversees the recruitment of participants and tracks the field site progress in order to ensure enrollment timelines are met. Coordinated centralized training for all site RAs as well as ordering the same equipment at each site as needed. Intimately works together on the sIRB application.
Carotid Reading Center
Responsible for carotid ultrasound training and certification for all RAs study-wide, reading of the carotid studies and QC. To date, the center has read and delivered to the DMCC data from 2,665 carotid scans. Carotid scans are performed with the portable GE LOGIQ 3 BT12 B-mode Ultrasound System (GE Healthcare, Wauwatosa, WI) to measure common carotid artery (CCA), intima-media thickness (IMT), inter-adventitial diameter (IAD) and presence and severity of plaque, well established markers of vascular aging and risk of future cardiovascular disease (CVD) events. The same Visit 2 reading protocols will be used at Visit 3, including angle of interrogation, vessel landmarks, scanning and reading machine settings, and readers. In terms of harmonization with FHS, LLFS and FHS use similar CCA IMT scanning and reading protocols.
Cognitive Reading Center
Oversees the selection, standardization, implementation, and data harmonization with FHS (and other studies where possible) of all cognitive assessment procedures. Table 1 outlines the collected data with asterisks indicating tests that capture digital data with the electronic pen and digital voice recordings, offering greater sensitivity for subtle errors at the upper end of cognitive functioning. All cognitive measures acquired in LLFS are identical or directly comparable to those collected in FHS. In the case of verbal list learning, where two different tests are used, generalizable memory scores (e.g., learning slope, percent retention) will be calculated and used to compare across cohorts. In addition to cognitive testing, measures of everyday functioning and instrumental activities of daily living (IADLs) are collected via the Clinical Dementia Rating (CDR) Scale, the Dementia Questionnaire (DQ), and the Lawton and Brody ADL scale, all of which will be used to inform the newly proposed dementia review. To maintain consistent standards of QC, at the start of each data collection cycle, all research assistants (RAs) undergo testing certification and annual re-certification by Dr. Stephanie Cosentino, a clinical neuropsychologist.
| Table 1. Cognitive Testing Battery | |
| Test | Primary Domain |
| MMSE* | Global Cognition |
| WMS-R Logical Memory ** | Verbal Episodic Memory |
| Digi Span Forward/Backward** | Attention and Working Memory |
| WMS-R Digit Symbol* | Processing Speed |
| Animal Fluency** | Semantic Knowledge |
| Trail Making Test A* | Processing Speed |
| Trail Making Test B* | Exec Fxn: Set Shifting |
| Letter Fluency** | Exec Fxn: Generation |
| Digital Clock Drawing* | Multidimensional |
| HVLT-R** (CERAD in FHS) | Verbal Episodic Memory |
| Tests using the *digital pen and **digital voice in LLFS and FHS | |
Specific Aim 2 of the Phenotypin Core, supporting Project Aim P1a, is to rule in/out probable AD and other dementias in LLFS participants in accordance with the FHS dementia review procedure, integrating cognitive and functional assessments with all relevant medical records. Each week, the Dementia Review Panel will select participants for dementia review based on the presence of at least one of the following two diagnostic triggers at Visit 3: 1) CDR Global Score > 0; or 2) report of a cognitive problem by an informant on the Dementia Questionnaire (DQ). The dementia review procedure will include a request of all available relevant medical records including neuroimaging scans to inform the diagnosis. Criteria for dementia will be as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM) V. These criteria require cognitive impairment sufficient to cause a change in social or occupational functioning. As is common practice, the last criterion will be operationally defined primarily as a CDR score >=1 and/or evidence of cognitively-based functional impairment as ascertained through the other measures of IADL functioning. Criteria for specific disorders include, among others: Alzheimer’s Disease, Lewy Body Dementia and vascular dementia (with or without AD) for example. Diagnoses of Mild Cognitive Impairment (MCI) will be assigned when CDR = 0.5 and objective impairment is observed on cognitive testing. Dementia review will occur via weekly telephone conferences attended by a neuropsychologist (Stephanie Cosentino), LLFS neurologist (Lawrence Honig), behavioral neuroscientist (Stacy Andersen), and epidemiologist (Diane Ives). This team is well suited to carry out the dementia review. Dr. Cosentino leads 6 dementia diagnostic consensus conferences at CU, Dr. Honig is the long-time director of the ADRC Clinical Core at CU and works closely with Dr. Cosentino to assign dementia diagnoses in this capacity. Dr. Andersen specializes in neuropsychological assessments of long-lived individuals and will regularly attend FHS dementia diagnosis conferences to maintain harmonization of procedures between the studies. In the last year of the LLFS’s current funding, Drs. Cosentino and Andersen received an administrative supplement to carry out the Dementia Review protocol retrospectively, for all subjects seen in Visit 2 meeting the above stated criteria to trigger a review.
Regarding the use of digital pen technology, this was adopted by the FHS to more comprehensively quantify written responses by substituting use of a regular ballpoint pen with a digital pen first for the Clock Drawing Test and then extended to all tests that require written responses. Both the digital voice and digital pen data allow collection of decision-making latencies and characteristics that may also reflect subtle differences in underlying cognitive processing. The digital pen Clock Drawing Test (dCDT) permits precise, reliable, and objective assessment of key cognitive constructs. Using proprietary software developed by MIT and Lahey Clinic, metrics were noted potentially sensitive to neurocognitive decline. In another FHS effort led by Dr. Rhoda Au, a new proposed collaborator with this application, digital voice recordings of verbal tests produced an average AUC of 0.76 in diagnosing AD. Adding natural language processing (NLP) based features boosts the value to 0.91 (prelim data presented at 2018 Alzheimer’s Association International Conference, Chicago).
While it would be ideal to include neuroimaging as part of the diagnostic process, LLFS participants are seen in their homes making this not feasible. This drawback will be partially mitigated by obtaining neuroimaging records when available and adding a thorough motor assessment to evaluate for stroke or Parkinson’s. Finally, validity of diagnoses will be assessed with the ~15% subsample of deceased participants (n=40) who will undergo post-mortem neuropathological study at Massachusetts General Hospital (MGH, see Neuropathology).
Morbidity and Mortality Committee
Performed a cause of death adjudication pilot project for University of Pittsburgh Field Center-based participants. The adjudication process was led by Dr. Joanne Murabito to harmonize with the FHS and is described in the LLFS Manual of Operations. Of the 428 deaths, 394 death certificates and 255 medical records were obtained; so far, 128 of the causes of death have been adjudicated (immediate, primary and contributing causes of death) in-person by 4 LLFS physician investigators. This has been particularly important for identifying dementia-related deaths which remain under-reported on death certificates. Given our experience, we are confident that this adjudication process can be performed for all deceased LLFS participants.
Neuropathology Assessments
For accurate diagnoses of dementia and likely dementia types, in addition to evaluation of clinical data, we are proposing to perform post-mortem brain collection, neuropathological assessment and brain banking. Based upon the current proband mortality rates, we anticipate that over the 5- year period of the grant, at least 250 of proband generation participants will pass away. Based upon the NECS experience, we anticipate that ~15% or ~40 participants (8 per year x 5 years) will donate their brains for study. All older generation participants will be recruited for this effort. Once the person dies, a local diener will remove the brain and ship it overnight to the Massachusetts General Hospital Neuropathology Service (Matthew Frosch, MD). The service handled 984 cases last year. Neuropathological assessment is the definitive diagnostic method for a wide range of neurological diseases. Our primary focus will be on ruling in or out dementia and classifying the type of dementia (including mixed types). Dr. Frosch and a neuropathology fellow will work with the LLFS dementia review panel in conducting clinical-anatomical correlations. Half of the brain will be flash-frozen and half will be formalin-preserved and both will be bio-banked for future uses and sharing.
Pulmonary Reading Center
Train and certify the RAs study-wide for continued longitudinal collection of pulmonary function measures (FVC, FEV1 and FEV6) using the handheld EasyOne diagnostic spirometer as has been the case since the first home visit. FEV6 is used in lieu of FVC as FEV6 is easier to collect from members of this elderly cohort, thereby improving reproducibility and reducing participant burden. Quality control results, investigated across Visit 2 have demonstrated a solid consistency by all four Field Centers in terms of obtaining good quality control scores within a low number of test attempts. Results have far exceeded the desired 3.0 quality control code score. Additionally, test attempts to obtain this score averaged at 4.3 attempts, far below the eight attempts recommended to reduce participant burden. These results, alongside the value of obtaining longitudinal measures across three data points from a relatively inexpensive, efficient and safe procedure, support the continuation of pulmonary data collection.